Education about this is so very important, and we’ve got to spread the word.
So let’s jump in and talk broad brush strokes about what lymphedema is, how signs and symptoms often appear, and about some risk reduction practices.
The lymphatic system and lymphedema
Your lymphatic system is largely responsible for the fluid balance in your body, and it also plays a role in immune function. You can think of the lymphatic system like a kind of plumbing system. The tiny vessels pull excess fluid from your tissues and with that, they collect things like dead cells, bacteria, and waste products, transporting them to the lymph nodes to be broken down. This is all then sent to the cardiovascular system and then eventually your urinary system takes care of what excess fluid and waste products need to be eliminated.
When there is damage to the lymphatic system, this circulation can’t happen, and the result is a backup of this protein-rich fluid that instead of being exported to your venous system is now accumulating in the tissues. This can cause swelling and thickening of the skin.
Primary lymphedema occurs when the lymphatic system is malformed at birth, even though symptoms may not show up until puberty, during pregnancy, or even later. This can be hereditary or spontaneous. Secondary lymphedema occurs as a result of an external factor, the most common causes being mastectomies, lumpectomies with radiation and/or removal of lymph nodes that may cause damage to the lymphatic system.
In its very early stages, lymphedema can spontaneously resolve on its own, but the chance of it returning is always present. In later stages, lymphedema can be managed with tools such as manual lymphatic drainage (MLD), bandaging, compression garments, and diligent skin care, but there is no cure. Lymphedema is a life-long, chronic condition. Life-long .This is often not an easy thing to hear.
What are some of the signs?
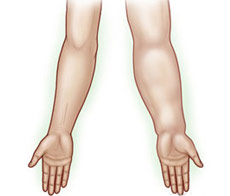
Symptoms can come on a few weeks after a procedure, or years later, or not at all. The onset of lymphedema can be gradual (which is most common), or it can sometimes come on quickly. Some symptoms may be felt before any swelling is ever actually visible, such as feelings of “heaviness” or “achiness” in the limbs. In the arms, it often starts in the forearm; and in the legs, it often starts in the foot or ankle area. It is also possible to develop lymphedema in the head, neck, or genital areas, though arms and legs are most common.
If swelling starts to become visible or noticeable (like suddenly your wedding rings stop fitting and you had a mastectomy on your left side), indentations that do not immediately disappear when you press in with your fingers (also called “pitting edema”) may be another sign, but this can vary as well.
If you believe you may be experiencing symptoms, contact your doctor for an evaluation and ask questions. A lot of questions, and don’t stop until you feel you are getting answers. I encourage you to ask lymphedema therapists in your area questions that you may be able to bring back to your doctor for clarification or ideas.
I’ve had a mastectomy/lumpectomy/radiation/node removal. How can I reduce my risk of developing secondary lymphedema?
Below are just a few of the risk reduction practices outlined by the National Lymphedema Network, reworded by me. For a full list sanctioned by the NLN, click here: https://www.lymphnet.org/pdfDocs/nlnriskreduction_summary.pdf
1. Your Skin
- Keep your skin protected to reduce the risk of infection. Keep the at-risk extremity clean and dry, and apply moisturizer daily.
- Avoid blood draws and injections on the at-risk limb.
- Wear gloves while doing activities that may cause injury to the skin. If you do get a scratch or puncture, wash it well with soap and water and watch closely for any signs of infection.
2. Exercise/Lifestyle
- Gradually build up the duration and intensity of any activity or exercise, and take frequent rest periods during activity to allow the at-risk limb to recover. For a position paper on exercise from the NLN, click here: https://www.lymphnet.org/pdfDocs/nlnexercise.pdf
3. Avoid Limb Constriction
- Avoid having blood pressure taken on the at-risk extremity , and wear loose-fitting clothing and jewelry.
4. Compression Garments
- Consider wearing a well-fitting compression garment for air travel. The decrease in cabin pressure puts stress on both the lymphatic and circulatory systems, and this can increase swelling.
5. Avoid Extreme Temperatures
- Avoid exposure to extreme cold, which can cause rebound swelling as well as chapping of the skin. Avoid prolonged exposure (more than 15 minutes) to heat, such as hot tubs or saunas.
The bottom line: Education is power. Spread the word about lymphedema . Mention it to your friends, your family, that woman in your dance class who just had a double mastectomy. Even though many people who have undergone things like surgery, radiation, or lymph node dissection will never develop it, it pays to know the ways to reduce your risk and the signs that can lead to early detection. Listen to your body, treat it with utmost care, and keep an open dialogue with your healthcare team.
Thank you for being an advocate for your health and for the health of those you care about.
Resources for further information:
National Lymphedema Network http://www.lymphnet.org/
Lymphedema Awareness Foundation http://www.lymphaware.org/
Step Up Speak Out (specific to breast cancer-related lymphedema) http://www.stepup-speakout.org/